Spinal cord injury (SCI) is a serious central nerve injury, which leads to partial or complete loss of sensory and motor functions below the injury level. After SCI, the primary injury and its secondary reaction lead to hemorrhage, immune reactions, cell death, and scar formation, and an inhibitory environment eventually develops in response to the injury, which inhibits neural regeneration. For patients with complete SCI, the sensory and motor functions below the injury level are completely lost and hardly recovered.
Recently, DAI Jianwu’s team from Institute of Genetics and Developmental biology, Chinese Academy of Sciences, in collaboration with Prof. ZHANG Sai’s group from Characteristics Medical Center of the Chinese People’s Armed Police Forces has confirmed the safety and preliminary effective of NeuroRegen Scaffold transplantation for spinal cord injury repair. Results were published in Science China Life Sciences (DOI:10.1007/s11427-021-1985-5).
NeuroRegen Scaffold (Image by IGDB)
Prof. DAI’s team has developed a novel linear-ordered collagen scaffold called the NeuroRegen Scaffold, which was able to guide neurite growth along its fibers and provided a "bridge" for spinal cord nerve regeneration. When these functional biomaterials together with neurotrophic factors or stem cells were transplanted into rat, canine or monkey models of complete transection SCI, they reduced the formation of the cystic cavity, reduced the deposition of regeneration inhibitory molecules at the injury site, and eventually promoted the recovery of motor function. Based on the preclinical studies, the first clinical research on NeuroRegen Scaffold transplantation for the treatment of complete SCI patients began in January 2015.
NeuroRegen Scaffold transplantation (Image by Xinhua)
Fifteen patients with acute complete SCI and Fifty-one patients with chronic complete SCI were followed up for 2-5 years. No serious adverse events related to functional scaffold transplantation were observed. Among the patients with acute SCI, five patients achieved expansion of their sensory positions and six patients recovered sensation in the bowel or bladder. Additionally, four patients regained voluntary walking ability accompanied by reconnection of neural signal transduction. Among the 51 chronic complete patients, 16 patients achieved expansion of their sensation level and 30 patients experienced enhanced reflexive defecation sensation or increased skin sweating below the injury site. Nearly half of the patients with chronic cervical SCI developed enhanced finger activity, and some patients showed the expansion of motor evoked potential spinal cord segments. Further analysis found that the recovery of sensory function was related to age, younger patients might be more likely to recover sensation after surgery.
This is the first large-scale, long-term study of NeuroRegen Scaffold transplantation to repair complete SCI. The results showed that NeuroRegen Scaffold transplantation is safe and preliminary effective in the treatment of acute and chronic complete SCI patients, and it brings the hope for the hopeless disease.
Contact:
Dr. DAI Jianwu
Institute of Genetics and Developmental biology, Chinese Academy of Sciences
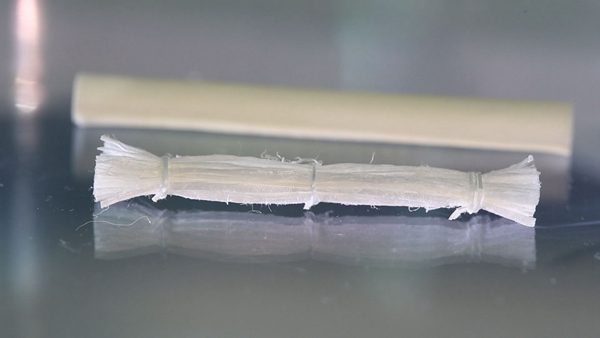 NeuroRegen Scaffold (Image by IGDB)Prof. DAI’s team has developed a novel linear-ordered collagen scaffold called the NeuroRegen Scaffold, which was able to guide neurite growth along its fibers and provided a "bridge" for spinal cord nerve regeneration. When these functional biomaterials together with neurotrophic factors or stem cells were transplanted into rat, canine or monkey models of complete transection SCI, they reduced the formation of the cystic cavity, reduced the deposition of regeneration inhibitory molecules at the injury site, and eventually promoted the recovery of motor function. Based on the preclinical studies, the first clinical research on NeuroRegen Scaffold transplantation for the treatment of complete SCI patients began in January 2015.
NeuroRegen Scaffold (Image by IGDB)Prof. DAI’s team has developed a novel linear-ordered collagen scaffold called the NeuroRegen Scaffold, which was able to guide neurite growth along its fibers and provided a "bridge" for spinal cord nerve regeneration. When these functional biomaterials together with neurotrophic factors or stem cells were transplanted into rat, canine or monkey models of complete transection SCI, they reduced the formation of the cystic cavity, reduced the deposition of regeneration inhibitory molecules at the injury site, and eventually promoted the recovery of motor function. Based on the preclinical studies, the first clinical research on NeuroRegen Scaffold transplantation for the treatment of complete SCI patients began in January 2015.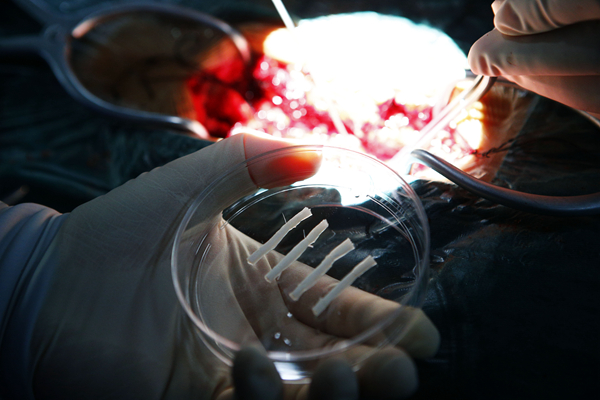 NeuroRegen Scaffold transplantation (Image by Xinhua)Fifteen patients with acute complete SCI and Fifty-one patients with chronic complete SCI were followed up for 2-5 years. No serious adverse events related to functional scaffold transplantation were observed. Among the patients with acute SCI, five patients achieved expansion of their sensory positions and six patients recovered sensation in the bowel or bladder. Additionally, four patients regained voluntary walking ability accompanied by reconnection of neural signal transduction. Among the 51 chronic complete patients, 16 patients achieved expansion of their sensation level and 30 patients experienced enhanced reflexive defecation sensation or increased skin sweating below the injury site. Nearly half of the patients with chronic cervical SCI developed enhanced finger activity, and some patients showed the expansion of motor evoked potential spinal cord segments. Further analysis found that the recovery of sensory function was related to age, younger patients might be more likely to recover sensation after surgery.This is the first large-scale, long-term study of NeuroRegen Scaffold transplantation to repair complete SCI. The results showed that NeuroRegen Scaffold transplantation is safe and preliminary effective in the treatment of acute and chronic complete SCI patients, and it brings the hope for the hopeless disease.Contact:Dr. DAI JianwuInstitute of Genetics and Developmental biology, Chinese Academy of SciencesEmail: jwdai@genetics.ac.cn
NeuroRegen Scaffold transplantation (Image by Xinhua)Fifteen patients with acute complete SCI and Fifty-one patients with chronic complete SCI were followed up for 2-5 years. No serious adverse events related to functional scaffold transplantation were observed. Among the patients with acute SCI, five patients achieved expansion of their sensory positions and six patients recovered sensation in the bowel or bladder. Additionally, four patients regained voluntary walking ability accompanied by reconnection of neural signal transduction. Among the 51 chronic complete patients, 16 patients achieved expansion of their sensation level and 30 patients experienced enhanced reflexive defecation sensation or increased skin sweating below the injury site. Nearly half of the patients with chronic cervical SCI developed enhanced finger activity, and some patients showed the expansion of motor evoked potential spinal cord segments. Further analysis found that the recovery of sensory function was related to age, younger patients might be more likely to recover sensation after surgery.This is the first large-scale, long-term study of NeuroRegen Scaffold transplantation to repair complete SCI. The results showed that NeuroRegen Scaffold transplantation is safe and preliminary effective in the treatment of acute and chronic complete SCI patients, and it brings the hope for the hopeless disease.Contact:Dr. DAI JianwuInstitute of Genetics and Developmental biology, Chinese Academy of SciencesEmail: jwdai@genetics.ac.cn CAS
CAS
 中文
中文




.png)
